
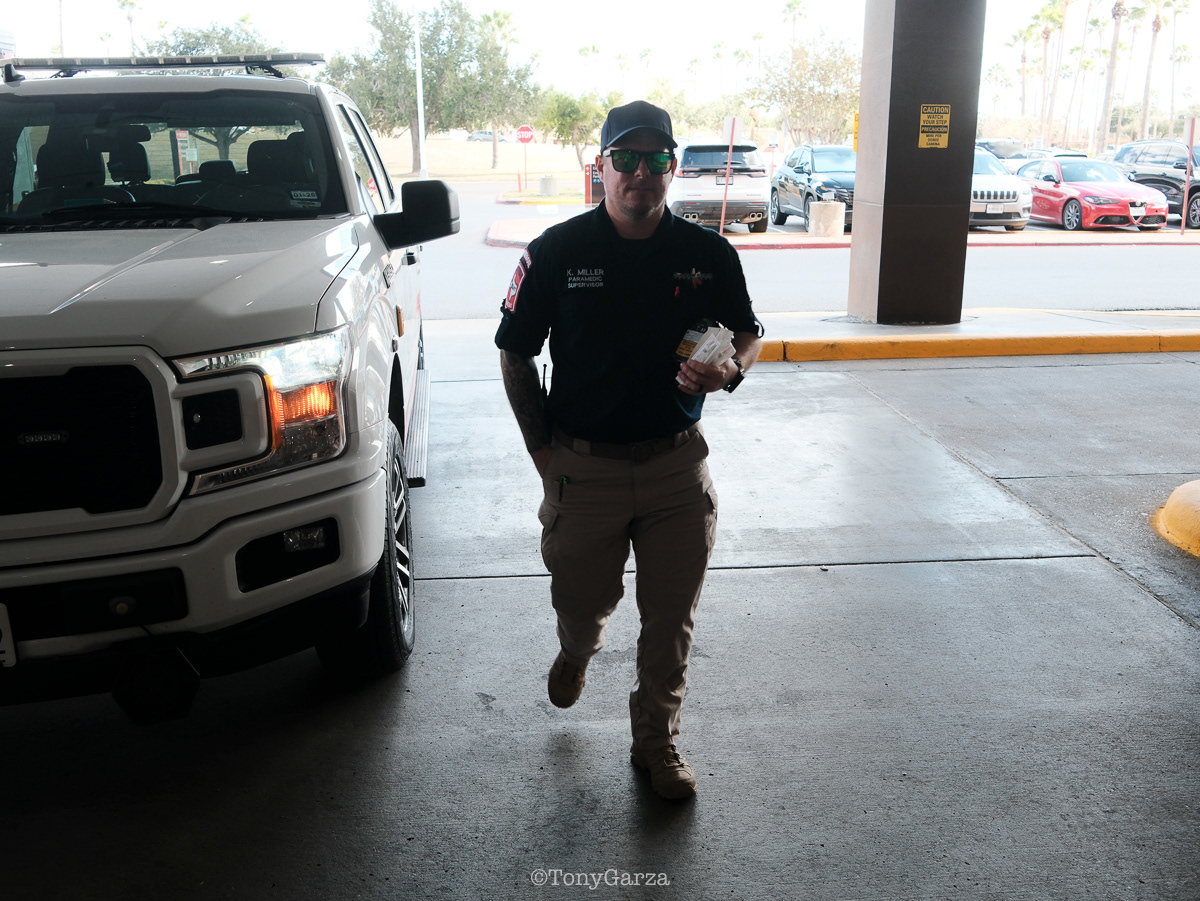
Rescue: Supervisor/Paramedic K. Miller, 12 years of experience in the field.

Rescue: Supervisor/Paramedic A. Garcia, 15 years of experience in the field.

Rescue: Supervisor/Paramedic O. Espinoza, 21 years of experience in the field.

Medic 4: Paramedic J. Pena and EMT S. Lopez,

Medic 7: Paramedic D. Garza and EMT Y. Lopez, over a decade of combined experience.

Medic 6: Paramedic R. Melchor and AEMT R. Chapa, combined experience of 8 years.

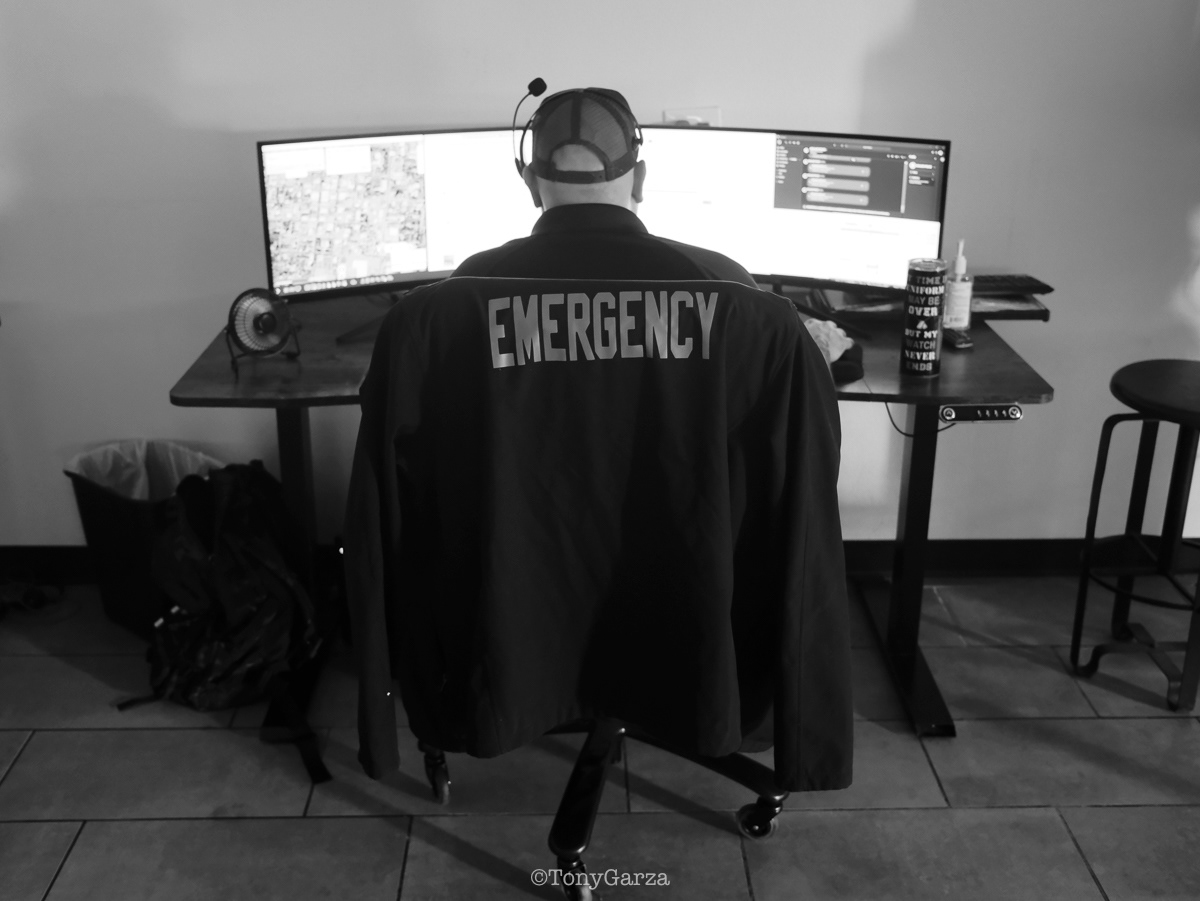
Dispatch: (Row 1) Alyssa, Daisy, Vanessa, Betina. (Row 2) Jose, Albert, Victoria, Omar, Caleb.
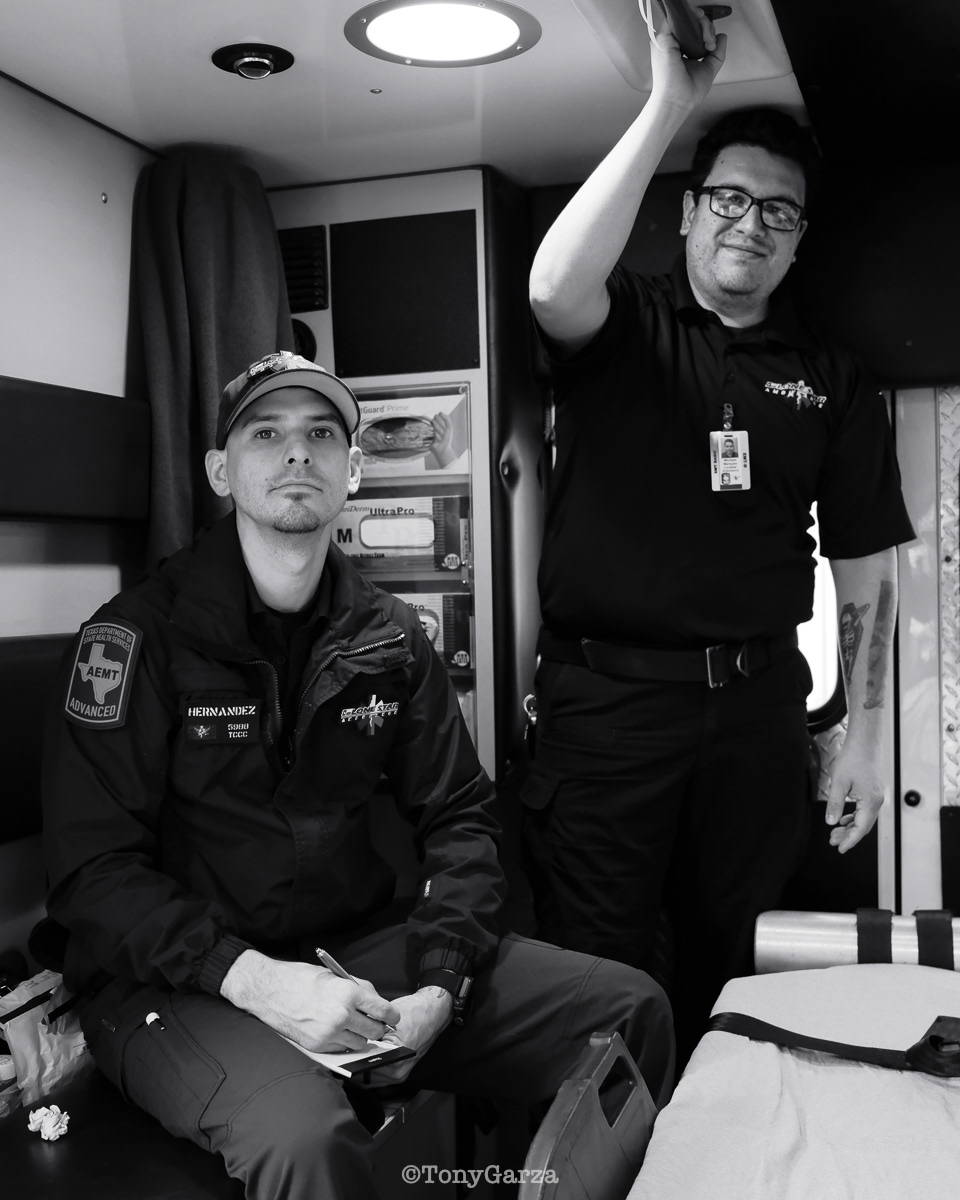
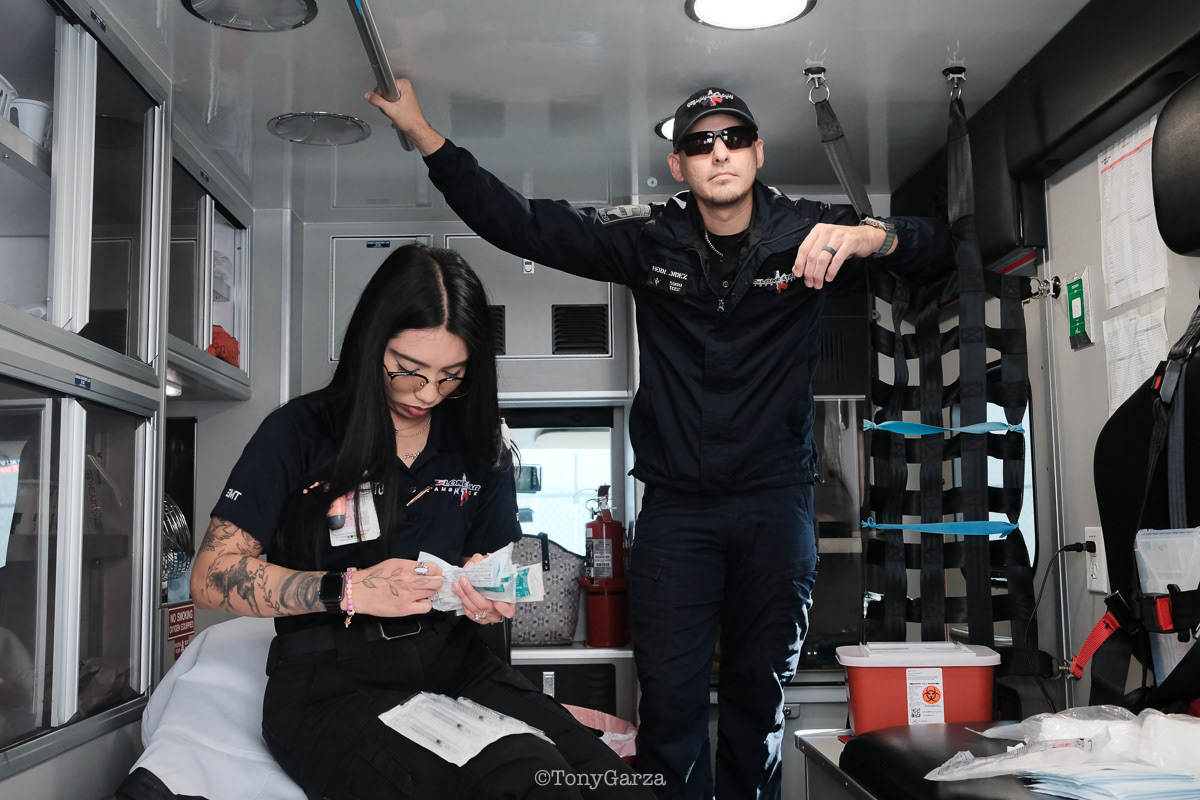
Alpha 3: AEMT J. Hernandez and EMT M. Marquez, on a 12 hour shift, with a combined experience of 22 years.

Alpha 2: AEMT M. Rodriguez and AEMT A. Pena. combined experience of 12 years.

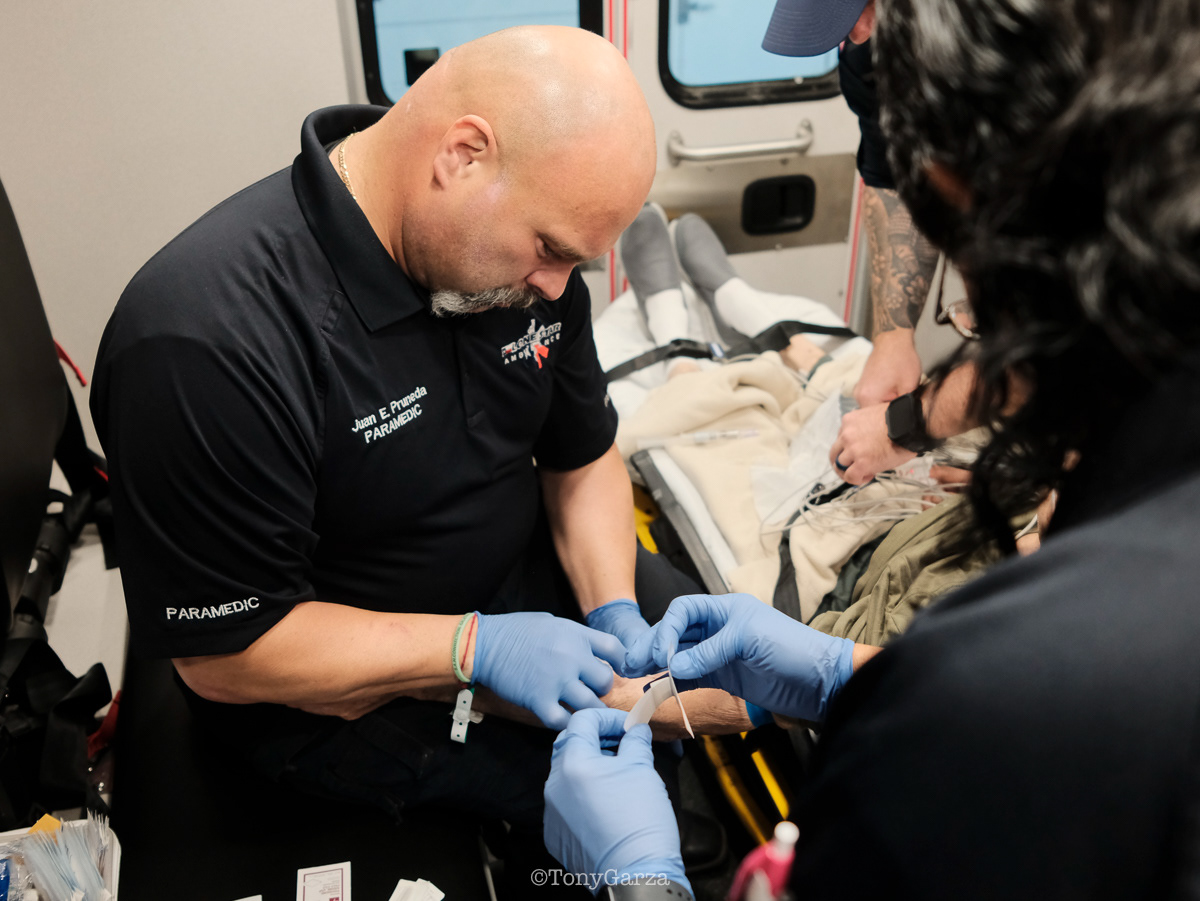
Medic 1: Paramedic J. Pruneda and EMT N. Dominguez, combined experience of 43 years.

Paramedic I. Valencia, on Medic 4, 3 years of experience in the field

Alpha 3: Paramedic R. Maciel (11 years) and EMT L. Ramirez (5 years), on a 12-hour shift, both joined EMS to get 911 experience and save lives.

Medic 11: Paramedic A. Munoz (6 years) and EMT L. Gaytan (14 years)

Medic 6: Paramedic R. Melchor ( 7 years) and EMT R. Longoria ( 6 years)

IFT Medic 32: EMT J. Hernandez and EMT A. Gomez

Medic 6: Paramedic J Amador (6 years) and EMT K. Zapata (3 years)

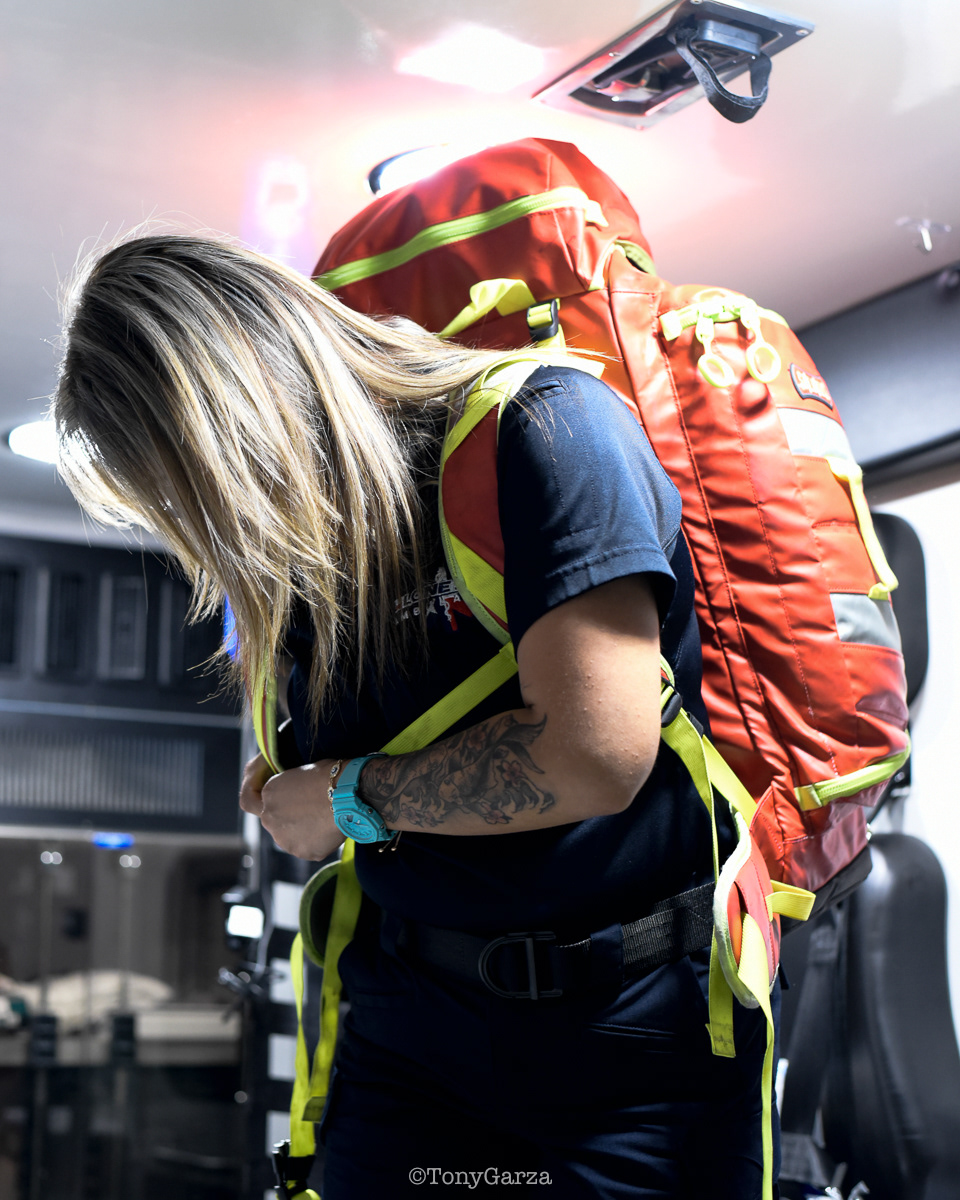
Rope rescue training with Lone Star Medics and McAllen FD.

Y. Lopez, EMT, with 9 years of EMS service

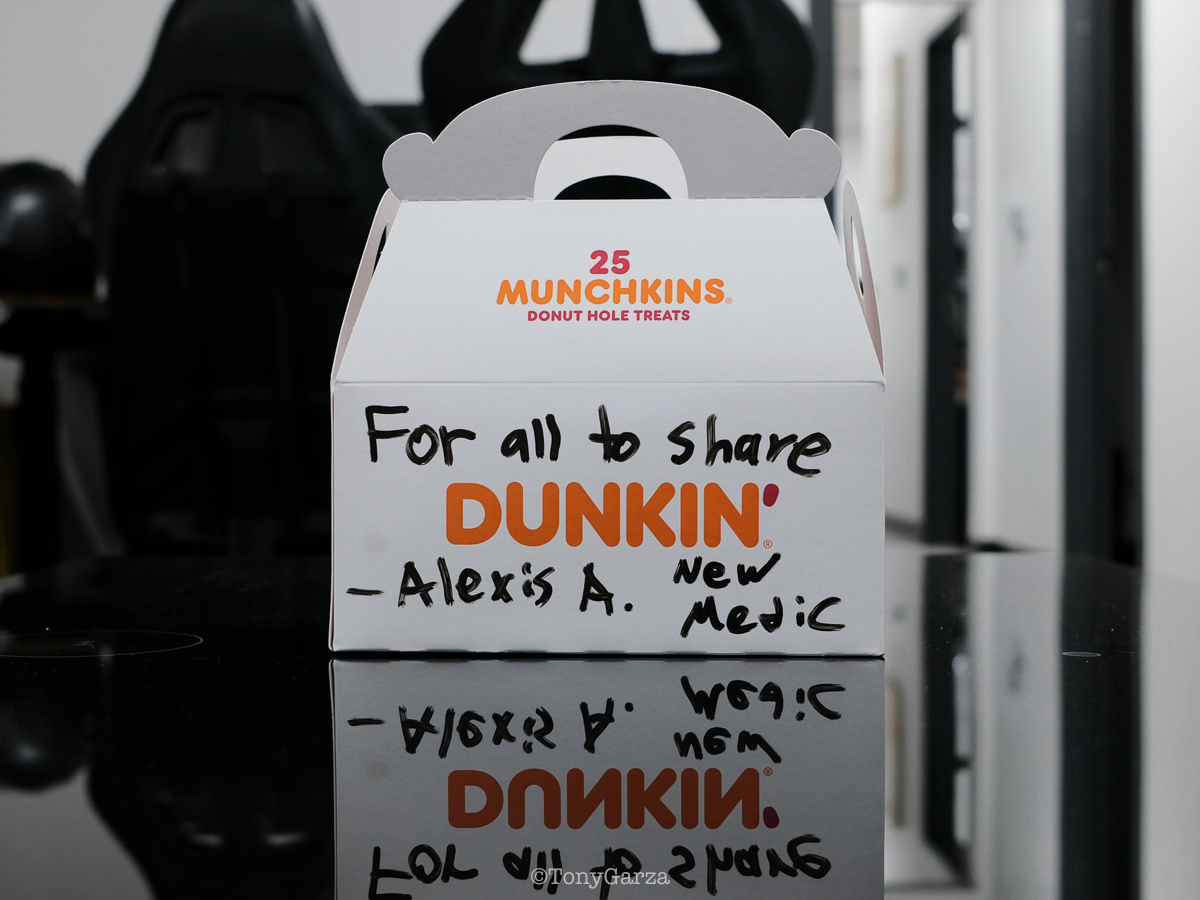
A. Cantu, EMT, with 2 months of EMS service.

R. De La Garza, Paramedic, with 4 years of EMS service.

K. Zapata, EMT, with 9 months of EMS service.

J. Pruneda, Paramedic, with 24 years of EMS service.

J. Pena, Paramedic, with 8 years of EMS service.

L. Gaytan, EMT, with 13 year's of EMS service

E. Hernandez, Paramedic, with 14 year's of EMS service.

S. Lopez, EMT, with 9 year's of EMS service.

E. Hernandez, Supervisor and Paramedic, with 10 year's of EMS service.

J. Lopez, Task Force Leader and EMT, with 21 year’s of EMS service.

G. Martinez, Director and Paramedic, with 13 year’s of EMS service.

C. Magallan, Dispatcher, with 2 year’s of communication services.

A. Rios, Dispatcher, with a year of communication services.

A. Ybarra, EMT, with 10 years of EMS service.

D. Garza, Paramedic, with 5 years of EMS service.

J. Casarez, Paramedic, with 4 years of EMS service.
Awards
& Honorable Mentions
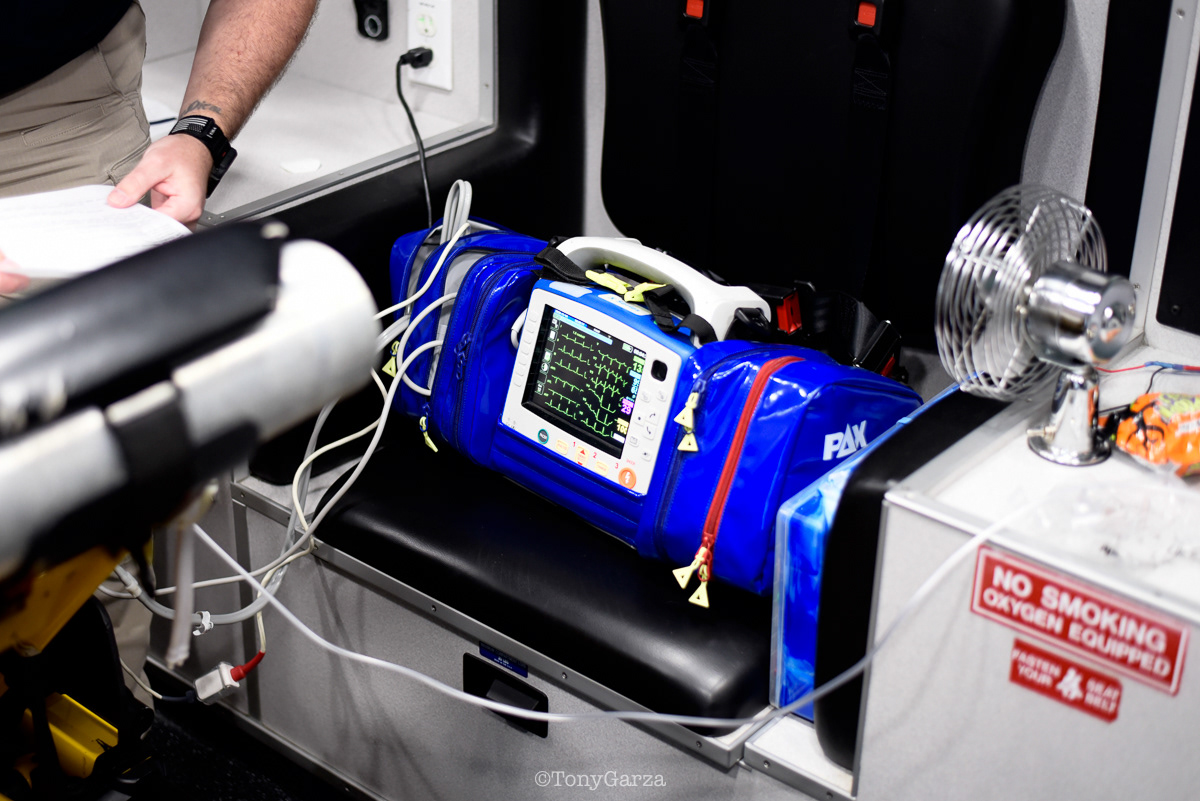
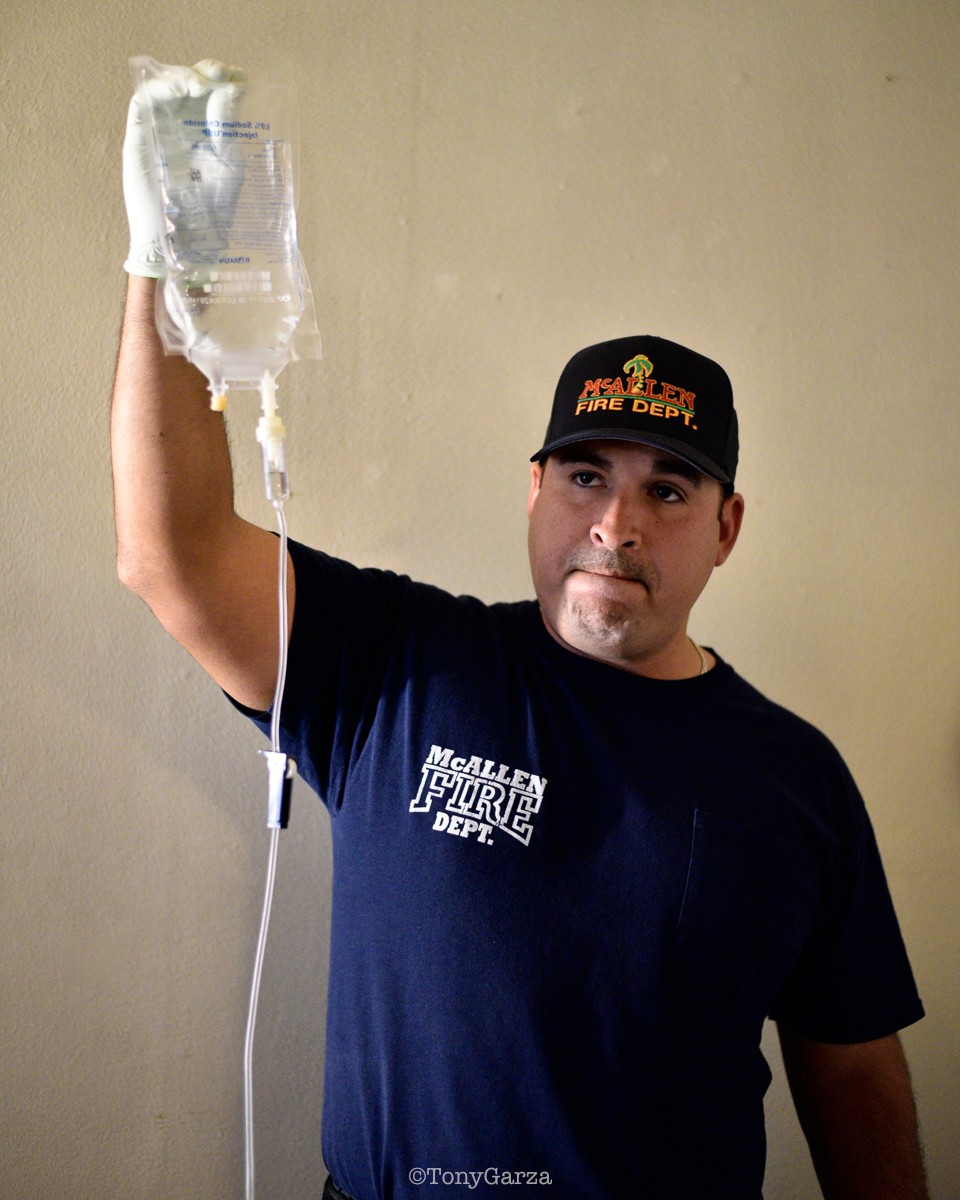
Rescue 1 is a single-paramedic unit: one supervisor/paramedic and one vehicle, with no stretcher and no extra hands. When all ambulances are committed, Rescue 1 is sent to the calls—heart attacks, major trauma, strokes, breathing problems, overdoses, and more.
With a monitor, jump bag, and medication kit, care begins immediately on scene. IVs, medications, 12-leads, airway support, decompressions, tourniquets, and blood are provided as needed. Rescue 1 keeps the patient stable until a transport unit arrives.
The mission is simple: save minutes, stabilize patients, and stay ready for the next call. The medic on Rescue 1 is highly skilled—rapid in action, decisive in treatment, and able to work under extreme pressure alone.
(Pictured: Supervisor/Paramedic O. Espinoza, with over 20 years of service, walking in and out from emergencies.)
With a monitor, jump bag, and medication kit, care begins immediately on scene. IVs, medications, 12-leads, airway support, decompressions, tourniquets, and blood are provided as needed. Rescue 1 keeps the patient stable until a transport unit arrives.
The mission is simple: save minutes, stabilize patients, and stay ready for the next call. The medic on Rescue 1 is highly skilled—rapid in action, decisive in treatment, and able to work under extreme pressure alone.
(Pictured: Supervisor/Paramedic O. Espinoza, with over 20 years of service, walking in and out from emergencies.)





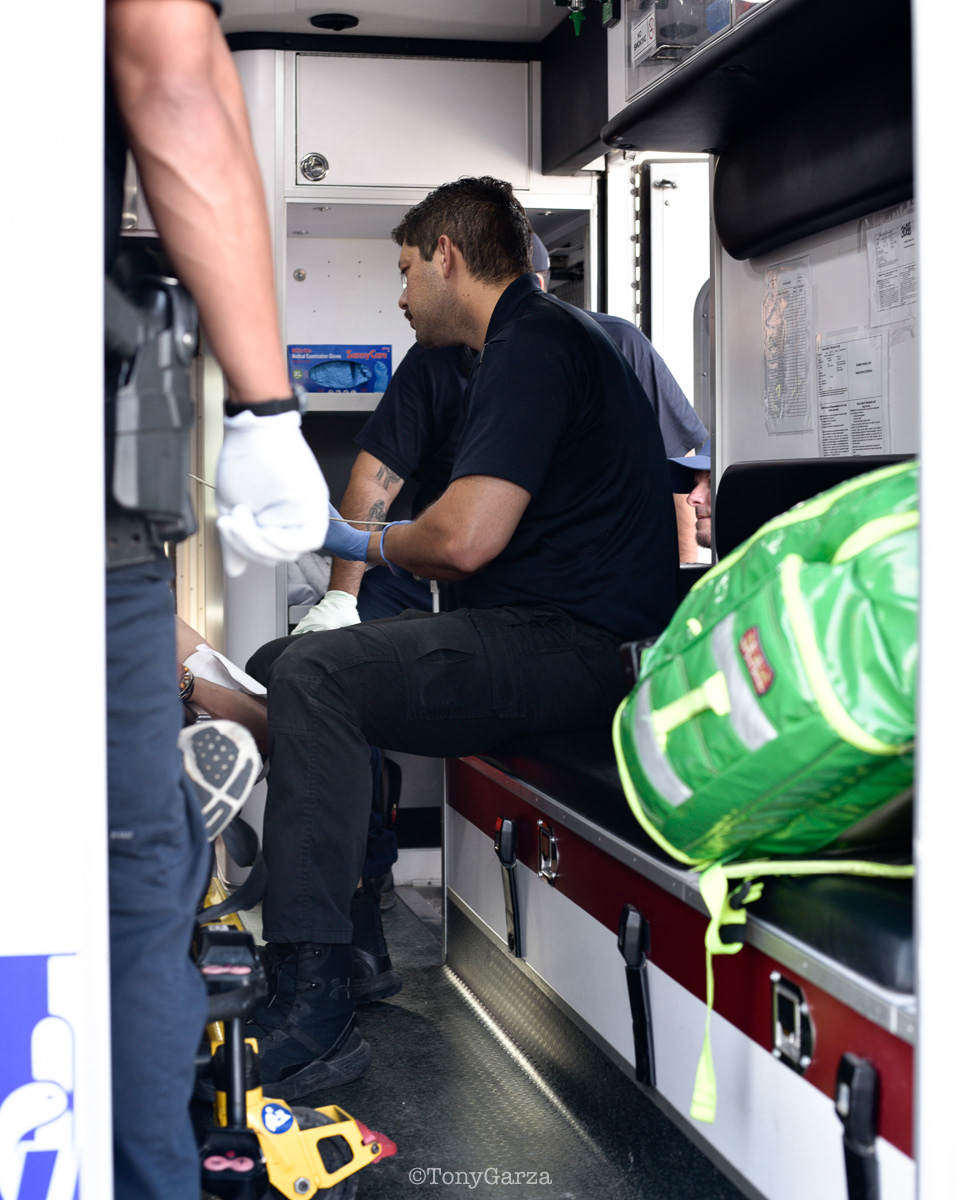
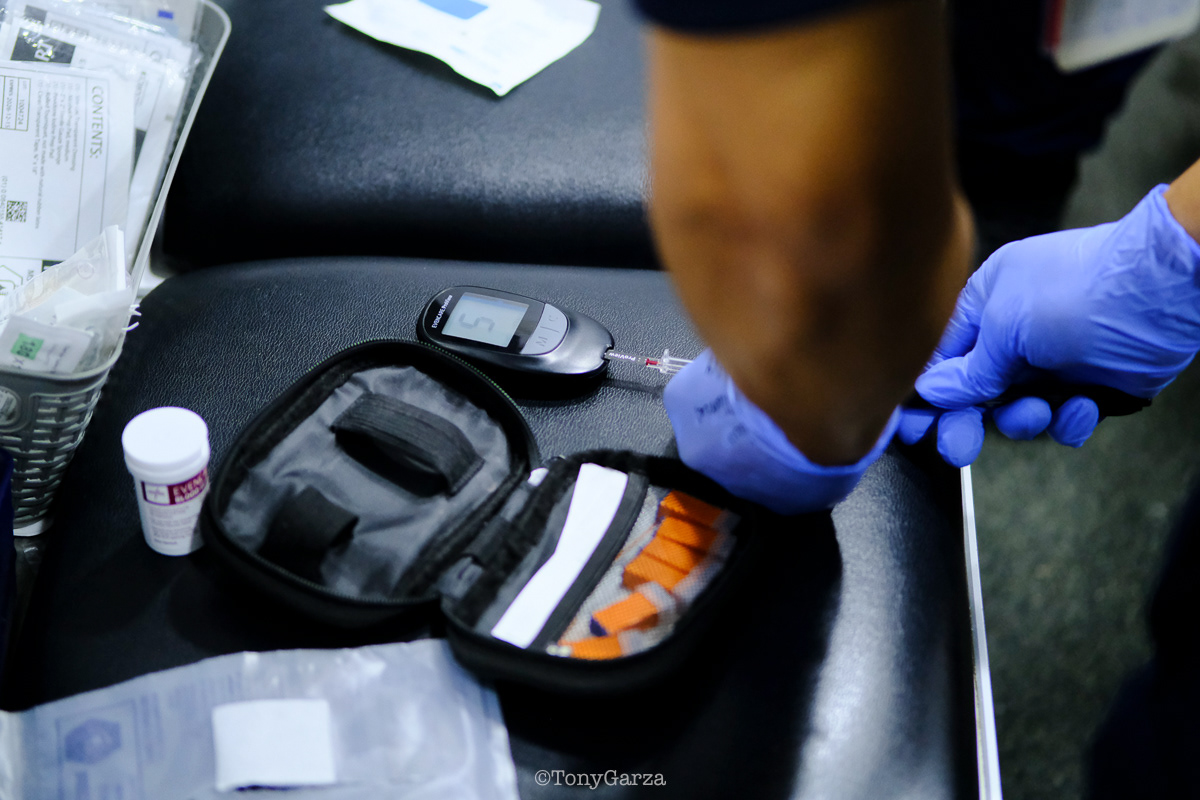
Medic 30 (Paramedic R. De La Garza/ EMT J. Hernandez) and Rescue 1 (Supervisor/Paramedic A. Garcia) responded to a sick call. Upon arrival, the team—led by Paramedic De La Garza—rapidly initiated assessment of the patient, who was presenting with vomiting and hypotension.
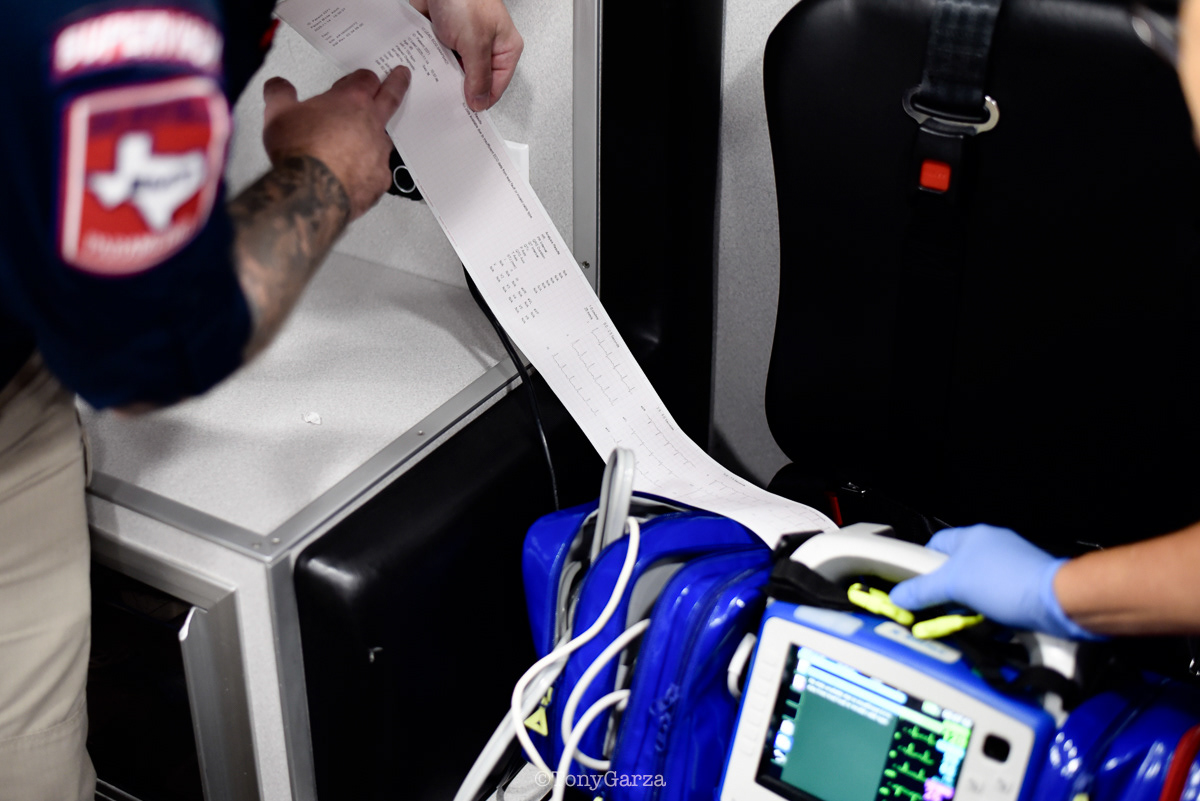
Once the patient was placed in the unit, Paramedic De La Garza performed a thorough yet rapid medical assessment and differential diagnosis, quickly identifying critical issues. She made sound clinical decisions and directed the team to initiate targeted interventions without delay, including obtaining vital signs, performing a 12-lead ECG, and establishing IV access, while she prepared the indicated antiemetic medication.
After completion of the 12-lead ECG and ruling out a heart attack, normal saline fluids were initiated and the medication was administered. The patient was promptly transported to the hospital of their choice. Paramedic De La Garza continued to closely monitor and reassess the patient en route, exemplifying strong leadership, clinical competence, and professionalism throughout the call.






Medic 6: Paramedic J. Amador sat beside the patient for the entire transport, making their comfort his priority. He demonstrated exemplary bedside manner as he carried out a thorough focused assessment, and asking clear, purposeful questions. His calm demeanor and steady, friendly conversation helped build trust. From the initial contact to hospital arrival, his attentiveness and professionalism were evident. Outstanding patient care.



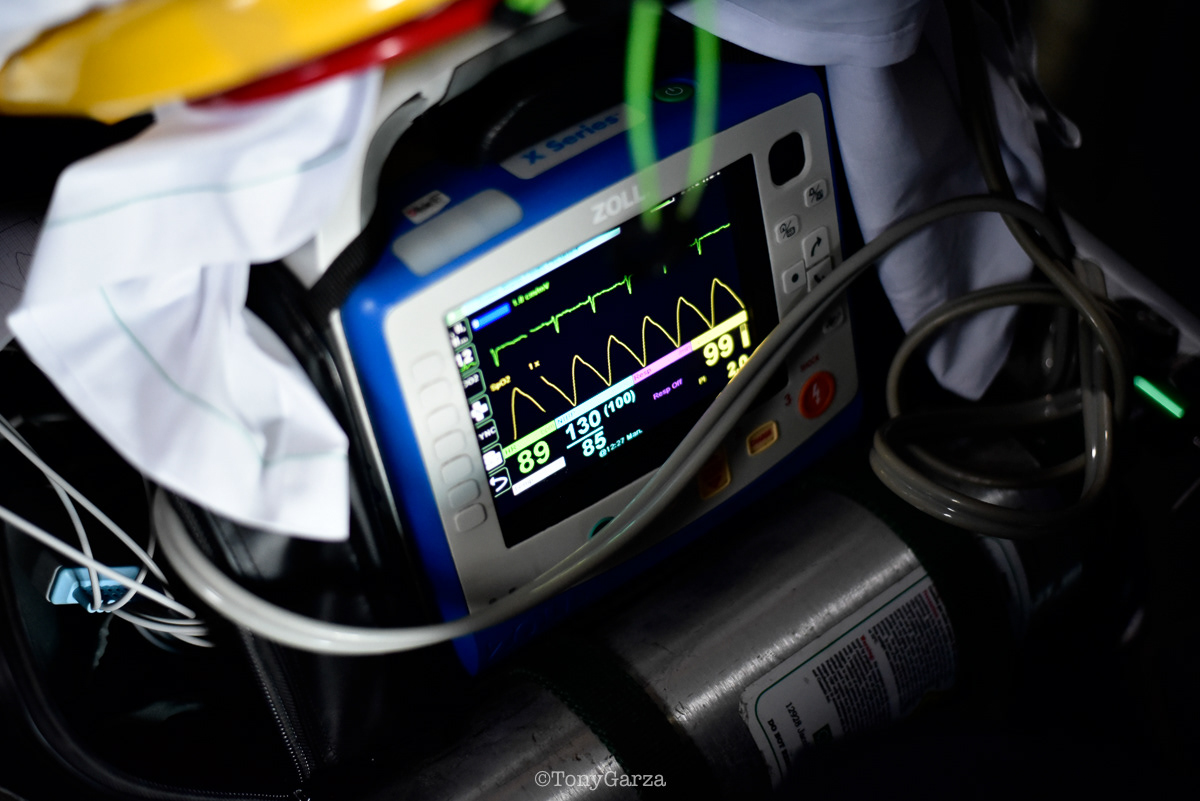

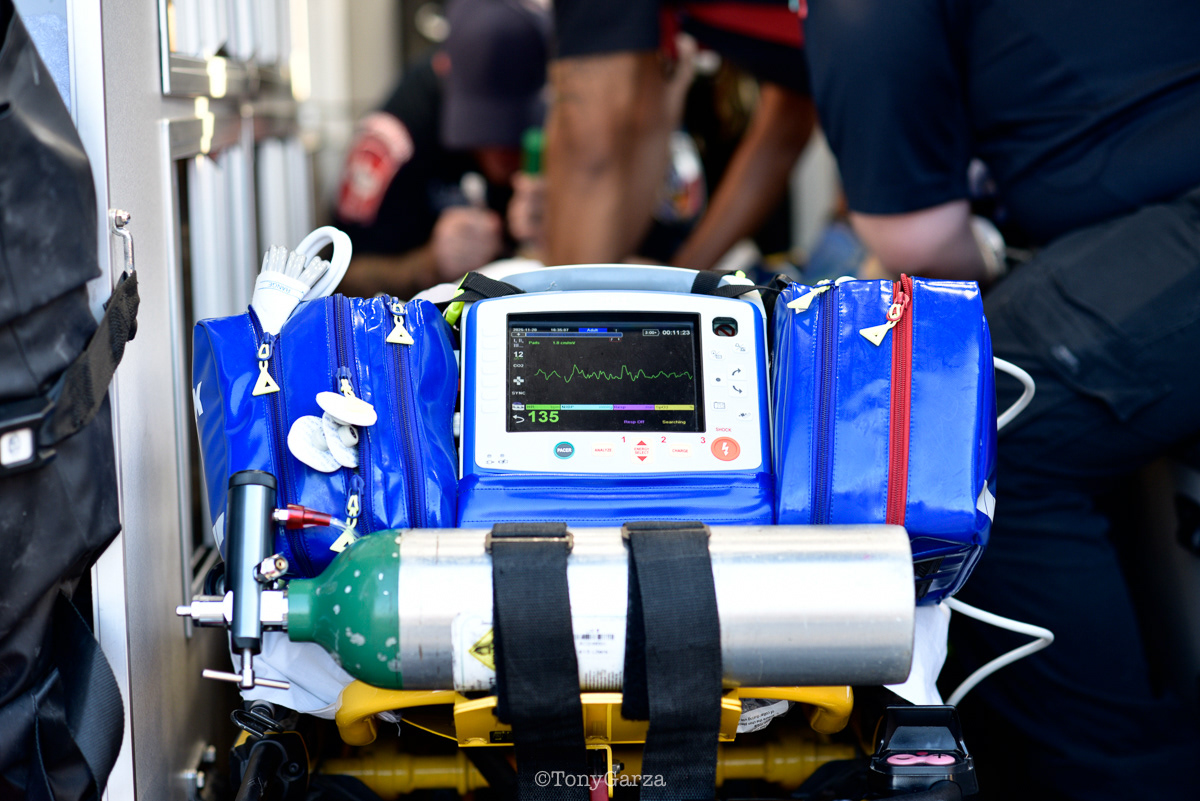
Medic 1 (Paramedic J. Pruneda and EMT N. Dominguez) and Rescue 1 (Supervisor/Paramedic K. Miller) performed an excellent differential diagnosis on a critically ill patient presenting with tachycardia and hypotension. Paramedic Pruneda quickly ruled out arrhythmia and myocardial infarction using ECG monitoring and a 12-lead ECG, narrowed the differential, identified the most likely condition, and initiated targeted treatment that effectively reduced the patient’s distress. Field differential diagnosis is a critical skill for paramedics, allowing them to tailor treatment to the most probable cause of a patient’s signs and symptoms. This approach ensures that simple, non-invasive interventions are attempted first, reserving more extreme measures for when they are truly necessary.
Outstanding work by Paramedic J. Pruneda, Supervisor/Paramedic K. Miller, and EMT N. Dominguez.



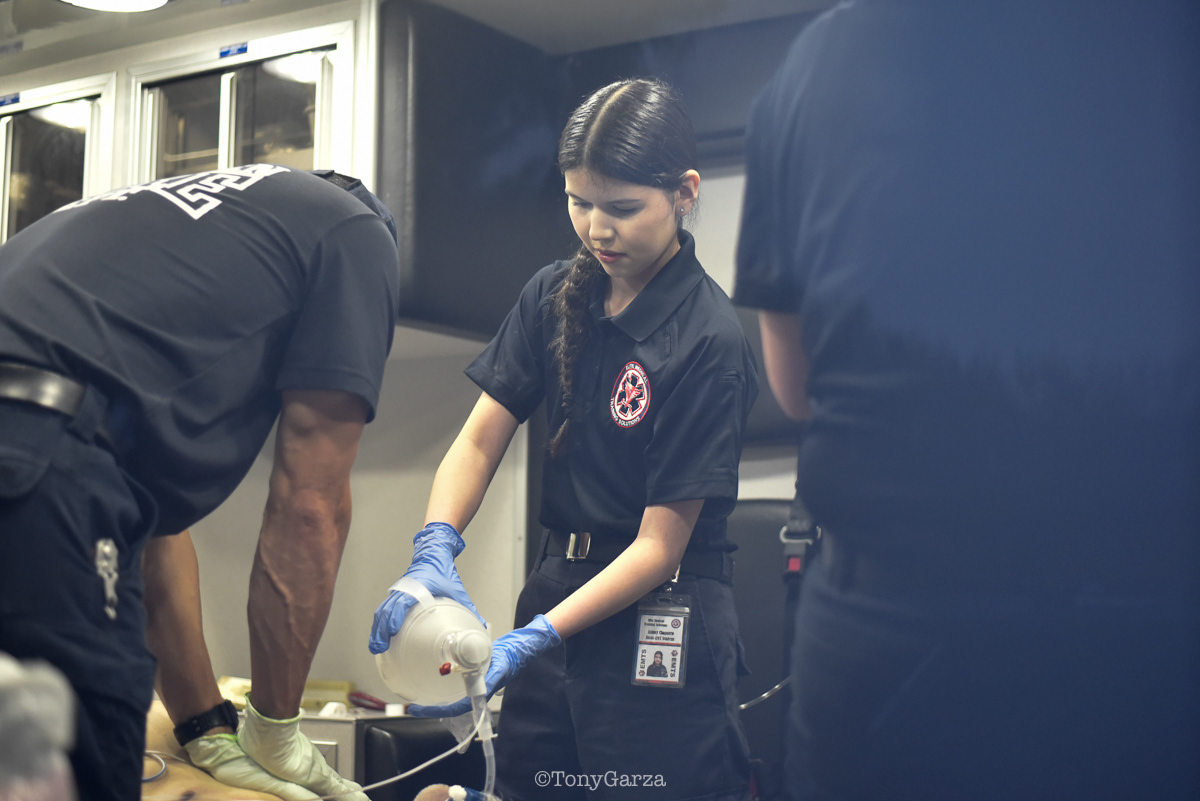
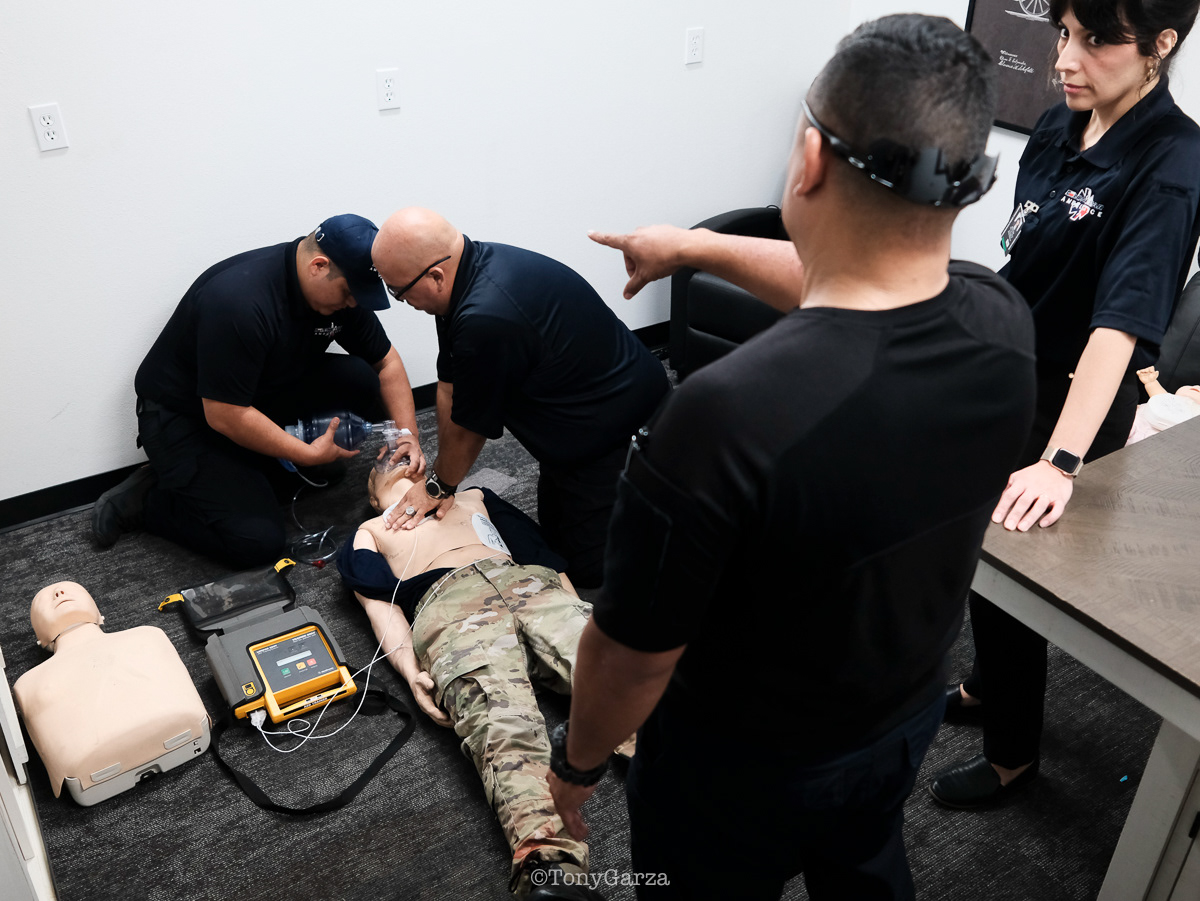
Medic 1 (Paramedic J. Anderson, EMT R. Longoria and EMT student A. Chaparro (first ride out, second arrest)), along with Rescue 1 (Supervisor/Paramedic A. Garcia), and McAllen FD, responded to a cardiac arrest. The crew intubated, established IV access, and administered cardiac medications on scene and en route. ROSC was achieved at the hospital. Great teamwork.



Rescue 1 (Supervisor/Paramedic K. Miller) responded to assist Alpha 1 (AEMT Ozuna and EMT Venecia) with an uncooperative patient requiring medical evaluation. Supervisor Miller effectively gained control of the scene, de-escalated the situation, and helped the patient calm down enough to voluntarily seek medical attention at the hospital.
Patient advocacy is one of the many critical responsibilities medics carry in the field beyond treating life-threatening emergencies. De-escalating an uncooperative or agitated patient is often more challenging than managing a full cardiac arrest; it requires patience, trust-building, and the ability to maintain safety while guiding the patient toward the care they need. This is textbook patient advocacy: recognizing that sometimes the most important intervention isn’t a medication or a procedure, but creating the conditions for someone in crisis to accept help. Good job to Miller and Alpha 1 for recognizing the need and requesting assistance.
Patient advocacy is one of the many critical responsibilities medics carry in the field beyond treating life-threatening emergencies. De-escalating an uncooperative or agitated patient is often more challenging than managing a full cardiac arrest; it requires patience, trust-building, and the ability to maintain safety while guiding the patient toward the care they need. This is textbook patient advocacy: recognizing that sometimes the most important intervention isn’t a medication or a procedure, but creating the conditions for someone in crisis to accept help. Good job to Miller and Alpha 1 for recognizing the need and requesting assistance.




Medic 6 – Paramedic R. Melchor and EMT R. Longoria saved the life of an elderly man in severe respiratory distress. The patient was alert and conscious but showing clear signs of hypoxia—slowly deteriorating with an SpO₂ reading in the 70s (normal >94%).
Acting quickly, Medic 6 delivered what may seem like simple but highly effective interventions: providing high-flow oxygen, administering medications to open the lungs, and applying CPAP to deliver continuous pressurized support. These treatments stabilized the patient, improved his oxygenation, and helped maintain his life during rapid transport.
Upon arrival at the hospital, the receiving team determined that intubation—the worst-case scenario—was not necessary due to the timely and skilled actions of Medic 6.





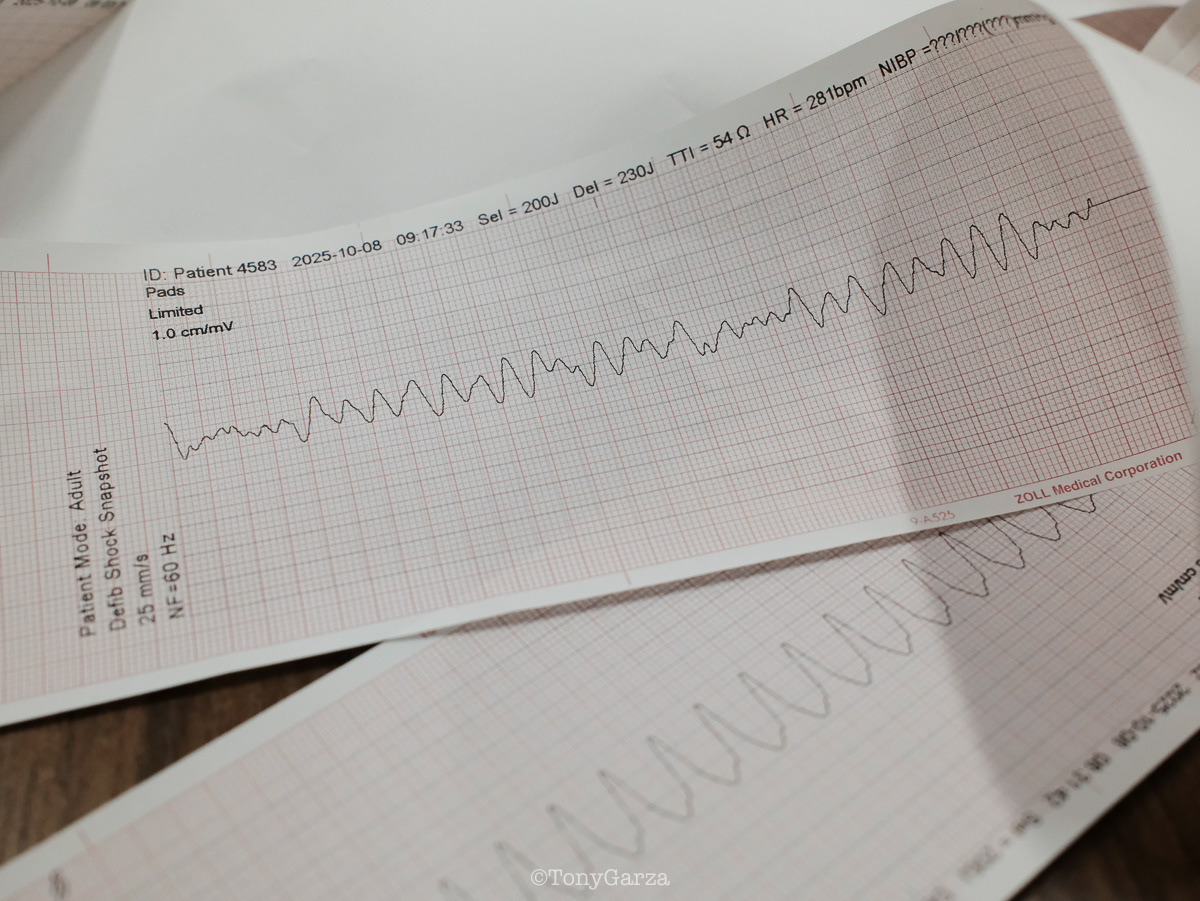
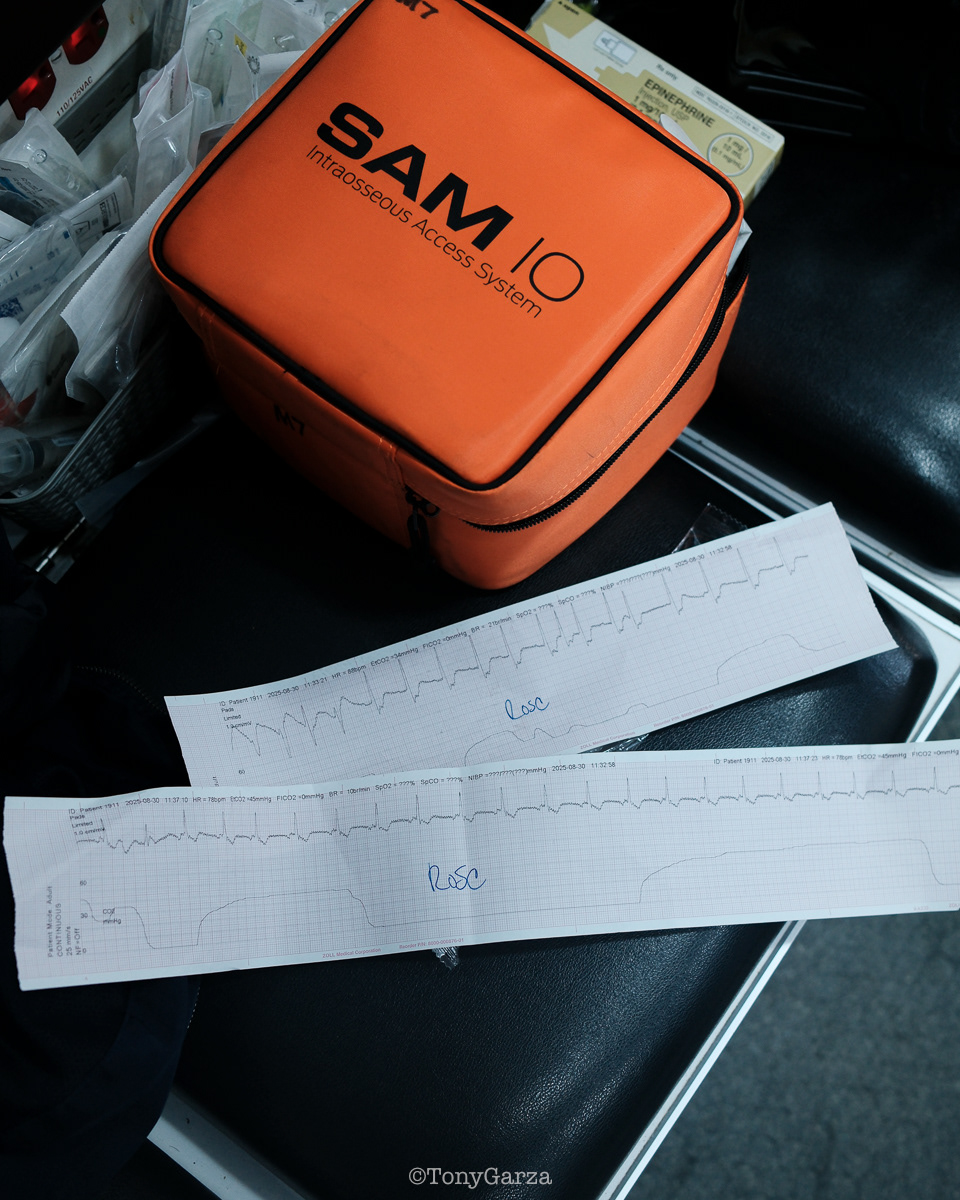
Medic 4: Paramedic J. Pena and EMT S. Lopez, assisted by Supervisor/Paramedic A. Garcia and McAllen Fire Department, respond to a cardiac arrest and achieve ROSC (return of spontaneous circulation) on location.








Medic 6: Paramedic M. De Pena and EMT R. Longoria, assisted by Supervisor/Paramedic K. Miller and the McAllen Fire Department, respond to a cardiac arrest. Pulseless, with some ECG rhythm changes, on scene and on the way to the hospital; ROSC was obtained at the hospital.




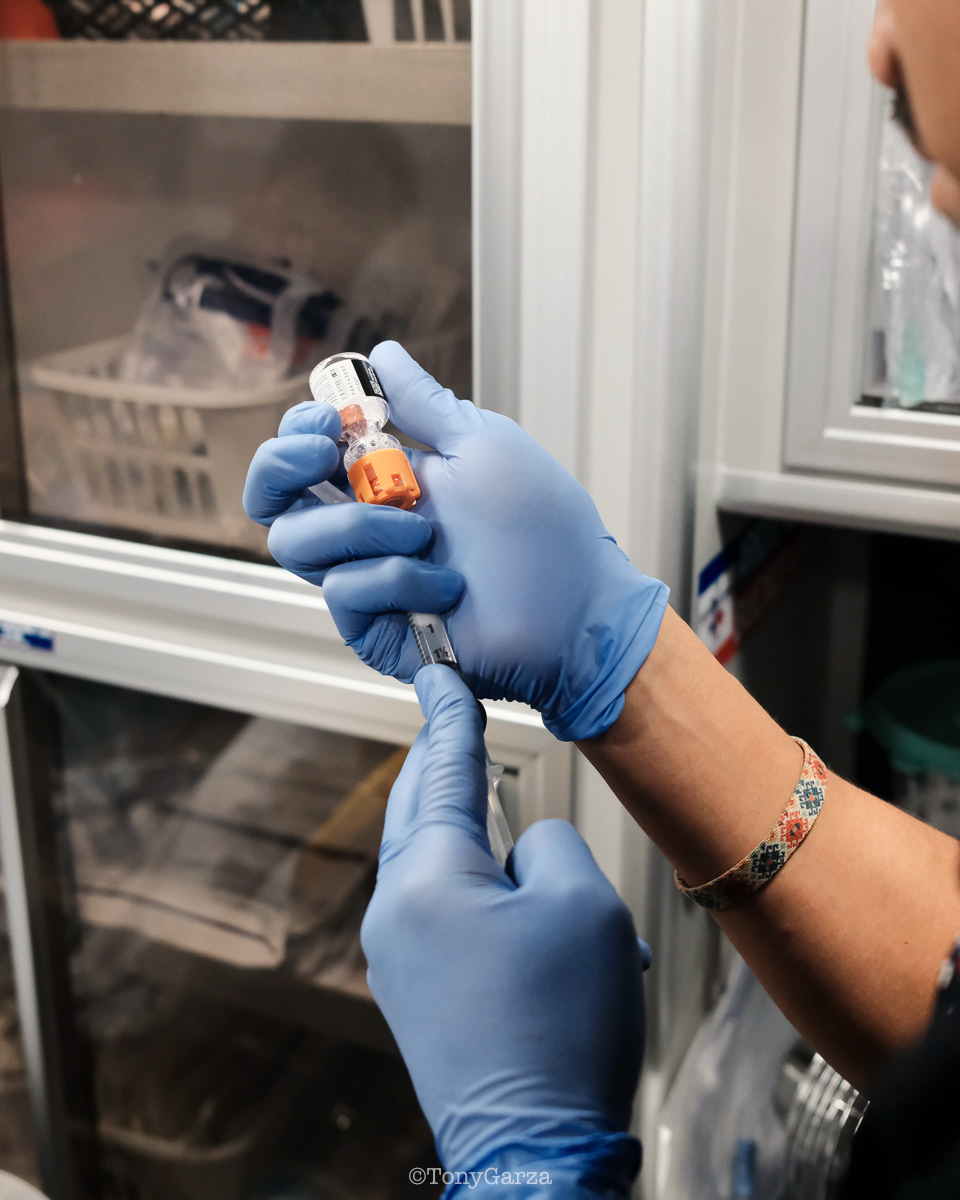
(first photo) Paramedic C. Rodriguez, on Medic 7, prepares antiemetic medication for a stroke patient experiencing slurred speech and nausea. The purpose is to relieve nausea and prevent vomiting that will compromise the airway during a rapid transport to the hospital. In making split-second decisions, field knowledge, experience, and foresight are critical.
(second photo) O. Espinoza, supervisor and paramedic, exits the unit after assisting Medic 7 with a critical call. Any additional assistance simply increases the chances for the patient. It’s not about ego, pride, title, or rank. Teamwork is dream work!


At the scene of a bee attack, Supervisor /Paramedic K. Miller is assisting the second patient in removing the bee stings that remain. If anaphylaxis occurs, it must be treated immediately since it is a life-threatening condition.
(History: In the early 1900s, anaphylaxis from a bee sting was recognized, and it was not until the mid-20th century that it was understood how to treat the life-threatening condition.)
(History: In the early 1900s, anaphylaxis from a bee sting was recognized, and it was not until the mid-20th century that it was understood how to treat the life-threatening condition.)


Medic 7—Paramedic D. Garza and EMT Y. Lopez—exemplify the qualities of an effective emergency response team. Each member understands their role and executes it with precision. Their coordination is so seamless that they often anticipate each other’s actions without speaking. This capability stems from countless hours spent working together, shared field experience, and a deep professional trust that allows them to function as one in the moments that matter most.





Doctor Robert Alejandro Cruz, along with DHR Health Neurology Department, present Lone Star Ambulance Paramedic E. Cordova, and EMT T. Tellez, with an award for their heroic act of helping and getting a stroke patient to the hospital. The patient received treatment in the appropriate time frame to have a full recovery.


Everyday EMS











After spreading Christmas cheer by delivering pizza to medics and dispatchers on duty, Supervisor and Paramedic A. Garcia took a moment to sit down and enjoy a meal, courtesy of LSA. Sincere appreciation is extended to LSA for their generosity and continued support of the crews.

































































































































































































EMS Philosophy

INTEGRITY- DOING THINGS THE RIGHT WAY KEEPS YOUR MIND CLEAR: ONE FOCUS. ONE WORRY—DOING IT RIGHT. DOING THINGS THE WRONG WAY. CUTTING CORNERS. IGNORING PROTOCOLS. WORRIES MULTIPLY. DO IT RIGHT. EVERY TIME. EVERY PATIENT. EVERY CALL. EVERY DECISION. IT’S THE STANDARD. IT’S THE WAY.
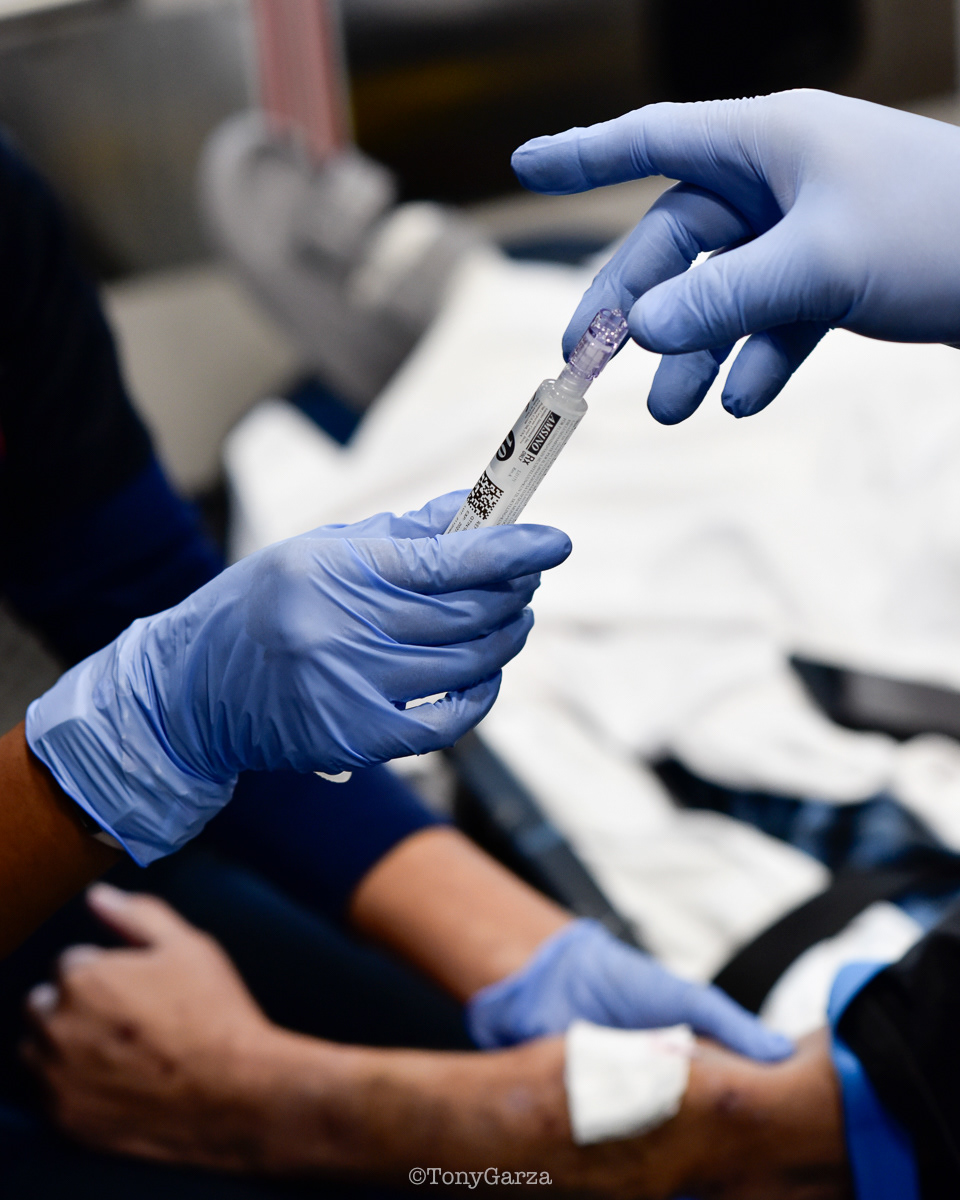
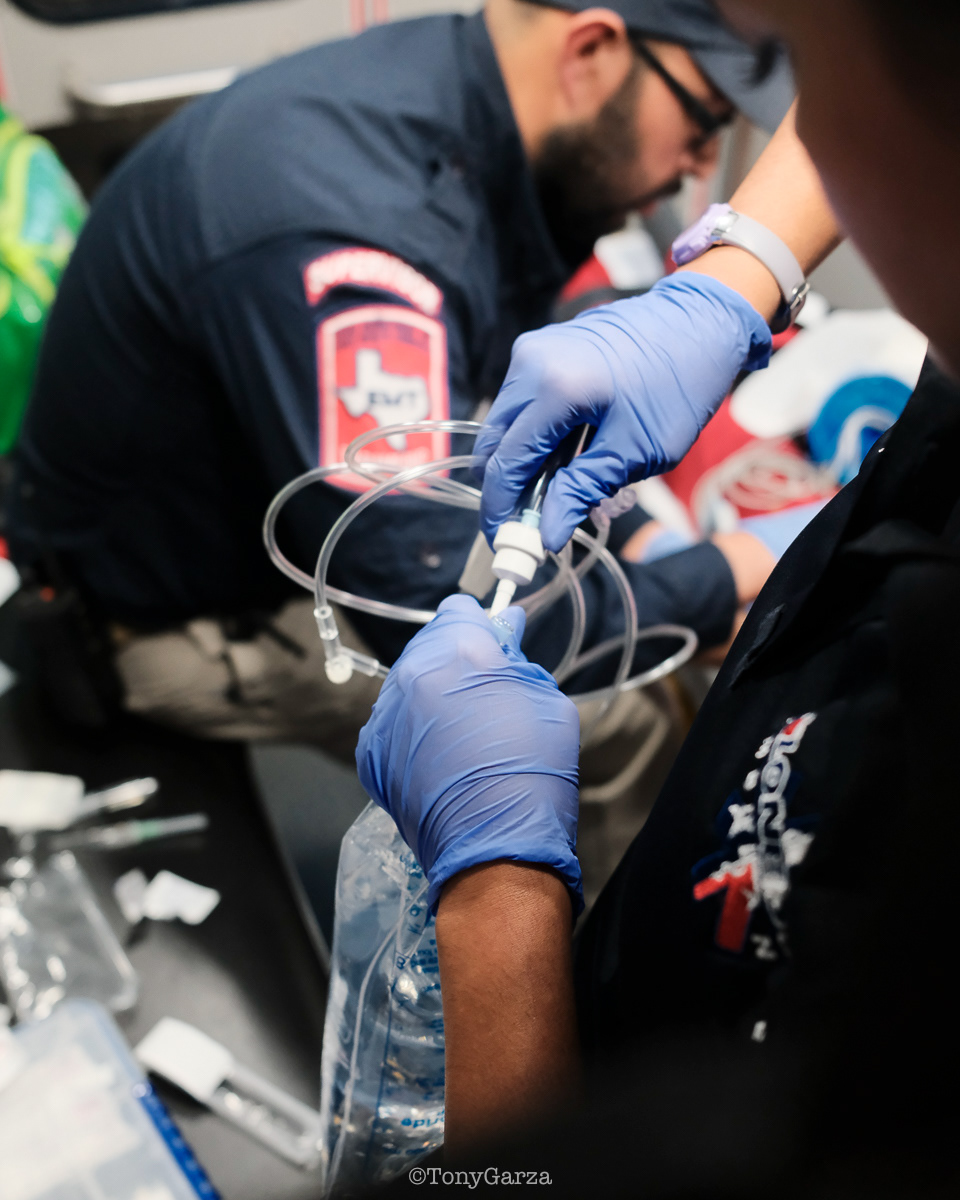
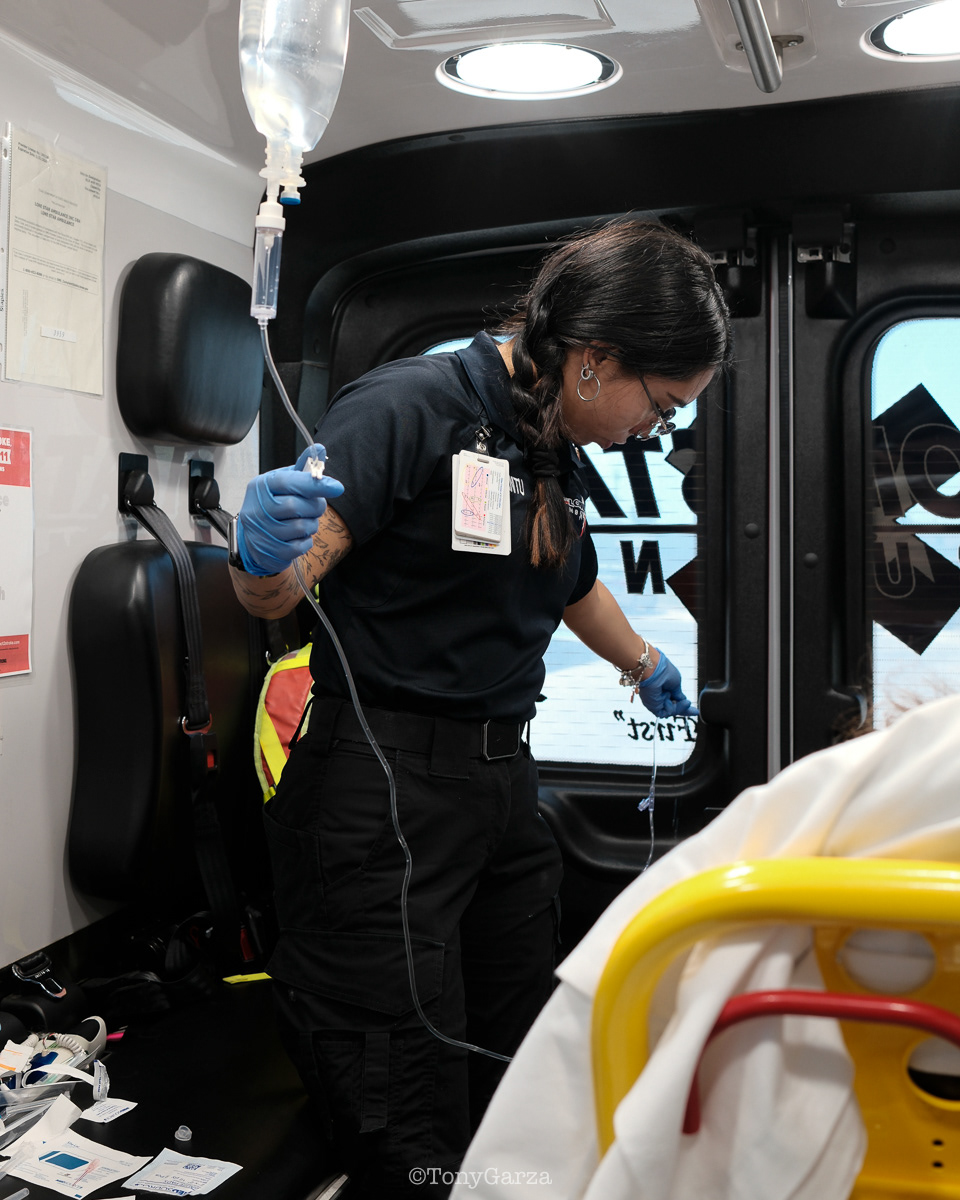
The Spark of Knowledge: Guided by seasoned paramedics, new medics learn emergency care as they enter and work in the field—a full-circle moment every medic experiences. Such mentorship is both a professional and ethical duty—essential and sacred. Its purpose is to pass knowledge from one generation to the next so the profession can advance, the highest standards of care are maintained, life is protected, and, above all, harm is avoided. All of this is possible only if the new generation understands and carries these principles forward. In this moment, the seasoned medic hands a filled NS syringe to the trainee, guiding them to complete the IV procedure—a spark of knowledge that creates a spark of life for the patient.

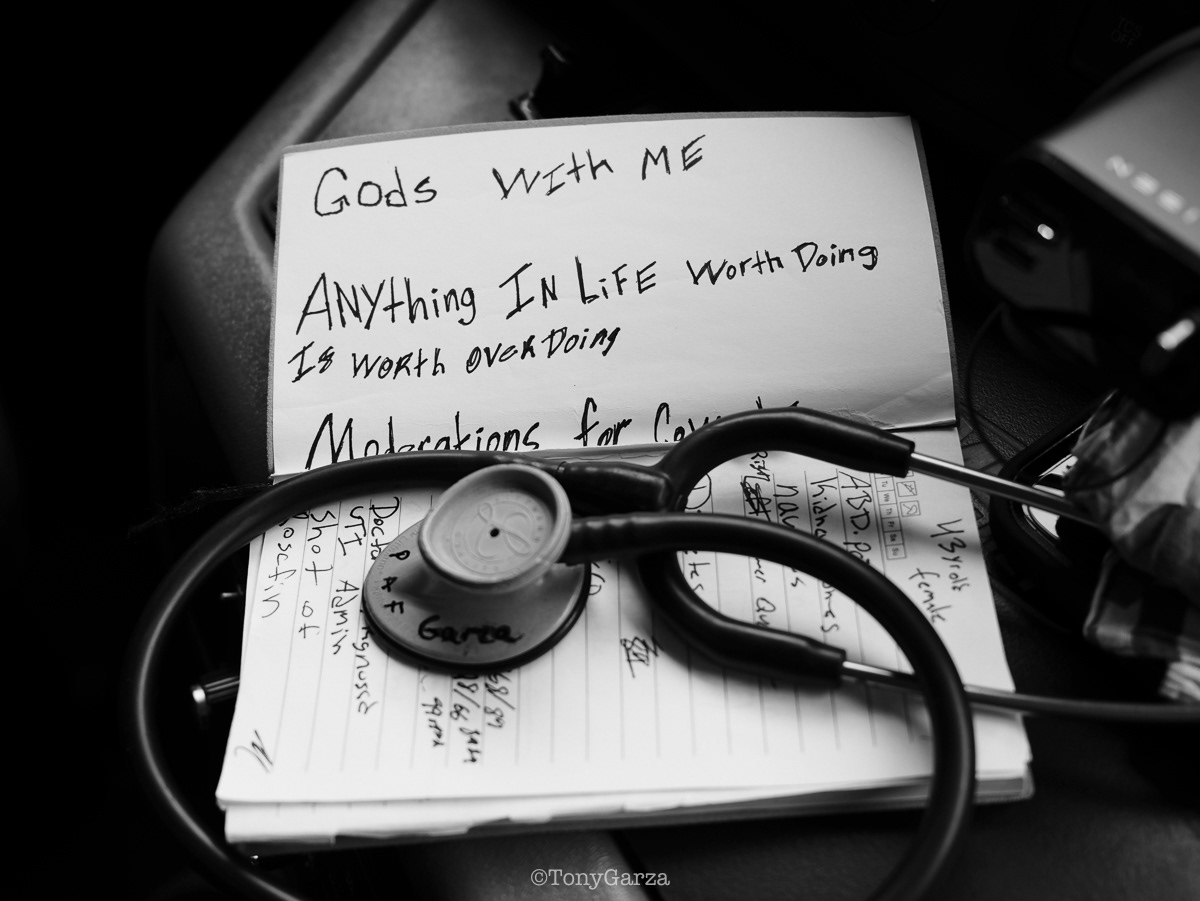
When you’re dying and you need a medic, which medic do you believe you deserve? A minimal-effort medic or a max-effort medic? Your answer to that question determines everything: • How you go about becoming a medic • How you show up as a working medic • How you live out your entire career as a medic Reflective questions like this one are used in EMS for a reason. They’re asked in class, during clinical, in the field, and after critical calls. They force you to be honest with yourself. They ask: “Am I truly living up to the standard I claim to uphold—the oath, the duty, and the honor?” Because max effort isn’t luck. It’s intentional. It’s disciplined. It’s the commitment to show up prepared, act decisively, continue learning, do the right thing, do no harm, and never cut corners. It’s the mindset that every patient matters, that you must do everything possible, that every call is someone’s life in your hands, and that your actions can make the difference between life and death. Max effort is a habit, a responsibility, and a standard you carry with pride—always striving to be the medic you would want saving you or your loved ones.

The Gathering: Before, during or after 12 or 24 hours A need to share What is seen What is death with. It’s necessary A psychological release To be ok To keep going To be human

Any comfort will help in a 24-hour shift. The inconvenience, if any, of carrying so much is outweighed by the benefits it provides to a medic on shift. Resting time, if any, even if only for 5 minutes, is essential and will be enhanced with the right comfort items. 5 minutes can feel like 30 minutes. No book, magazine, video, or photograph will ever show you this. To understand, you must experience it. You have to be in EMS.

A meal is more than just a meal for the medic; it means staying well so that others may live. Eating a meal not only gives one the energy to work long shifts, but it is also one of the simplest ways to boost morale, which is important in life and especially in demanding occupations. Although severe adversity helps to strengthen mental fortitude, excessive adversity can “burn out” even the most resilient minds. Morale is critical at that point. Most people outside of EMS can sit and eat a full meal uninterrupted, which has become an overlooked comfort. However, in EMS, it is a blessing.

Medics who serve on the front lines often become so exposed that they lose sight of the value of their role in society. This effect occurs naturally. Seconds and minutes are the battleground on which the war against illness and death is waged. It’s a beautiful war. Don’t forget that we are doing this so others may live.
